
iStock / krisanapong detraphiphat
The alcohol industry regularly spreads misinformation to obscure booze’s cancer link. Public health groups are demanding label warnings to give consumers clarity.
In retrospect, researchers Erin Hobin and Timothy Stockwell shouldn’t have been surprised that their first-of-its-kind experiment placing cancer warnings on 47,000 bottles of booze—funded by the Canadian government to the tune of $1 million (CDN)—got yanked.
Designed to assess the impact of eye-catching labels, researchers set out to affix bright yellow stickers bearing health messages onto nearly every alcoholic drink for sale at the sole liquor store in the city of Whitehorse, Yukon, for eight months. “It was a rare and unique opportunity,” said Hobin, a public health scientist for the province of Ontario, in a recent interview. But as soon as the experiment began in late November 2017, disgruntled emails from the heads of Canada’s beer, liquor, and wine lobby groups began to roll in. They demanded the Yukon government halt the study, according to public records the researchers later obtained—by Christmas, it was suspended.
Big Booze’s interference in what would have been an unprecedented study on alcohol cancer warnings is only one instance in a long history of efforts the industry has taken to sow doubt about drinking’s health effects. Other recent hits include the funding of flattering research and campaigns against policies that encourage drinking less. These actions muddy the general public’s understanding of how much it’s safe to drink—and in the cases of certain types of cancer, whether it’s safe to drink at all.
There is a frustratingly stubborn gulf between what experts know about alcohol’s cancer risk and the awareness of everyday drinkers.
Alcohol’s cancer link is irrefutable: In 1988, the World Health Organization (WHO) concluded that there is a causal relationship between ethanol—the specific type of alcohol in booze—and throat, liver, breast, and colon cancers. This link has since been acknowledged both by the Centers for Disease Control and Prevention—which advises that “for some conditions, such as certain types of cancer [for example, breast cancer] and liver disease, there is no known safe level of alcohol consumption”—as well as the U.S. Surgeon General, who has written that, “[for] breast cancer, studies have shown that even moderate drinking may increase the risk.” A public health analysis published last year estimated that the cancer risk posed by drinking one bottle of wine a week was comparable to smoking five cigarettes for men and 10 for women in the same time span.
In late October, eight organizations led by the Consumer Federation of America filed a petition to the Department of the Treasury’s Alcohol and Tobacco Tax and Trade Bureau (TTB), calling on the agency to set the record straight for consumers once and for all, by making explicit on all booze the fact that alcohol is a carcinogen. Since WHO’s declaration in 1988, our understanding of alcohol’s cancer risk has only become more clear, says Nigel Brockton, vice president of research at the American Institute for Cancer Research (AICR), one of the groups involved in the petition.
[Subscribe to our 2x-weekly newsletter and never miss a story.]
“Although the link between cancer and alcohol has been [noted] for 30 years, we see it in much finer resolution than we were able to before,” he said. But here’s the catch: Despite the scientific consensus, less than half of the general public knows that alcohol is a carcinogen.
“The tobacco industry pioneered this by manipulating the science on heart disease and cancer, by hiring researchers who pretty much get on their payroll and then create doubt about the linkages.”
Part of this, Brockton suspects, may be due to the myth that moderate drinking can be heart-healthy—an association that has long been debunked as a conclusion of shoddy analysis. Nonetheless, there’s a pervasive sense among the general drinking public that the science remains unsettled. That climate of doubt is no accident: A 2017 analysis found that industry-affiliated groups regularly spread misinformation online to cast uncertainty around alcohol’s cancer link. Companies also sometimes engage in a practice dubbed “pinkwashing,” which involves branding alcoholic products with ribbons denoting breast cancer awareness to obscure ethanol’s carcinogenicity. (In 2018, Mother Jones published a detailed investigation examining the efforts that the alcohol industry has taken to mislead the public about alcohol’s cancer link.)
As a result, public health advocates say, there is a frustratingly stubborn gulf between what experts know about alcohol’s cancer risk and the awareness of everyday drinkers. Cancer warnings are essential to closing that gap, said Thomas Gremillion, director of food policy at the Consumer Federation of America. Just take the impact of such labels on tobacco as an indication: Researchers have found that mandatory health messages are associated with increased knowledge about smoking’s risks, and that graphic warnings illustrative of particular risks like brain damage and cancer may increase interest in quitting.
“On the one hand, you have this huge contribution of alcohol to cancer and the public health burden, and on the other hand, you’ve got a majority of Americans for whom alcohol as a cancer risk is not on their radar,” Gremillion said in an interview. “They don’t put two and two together.”
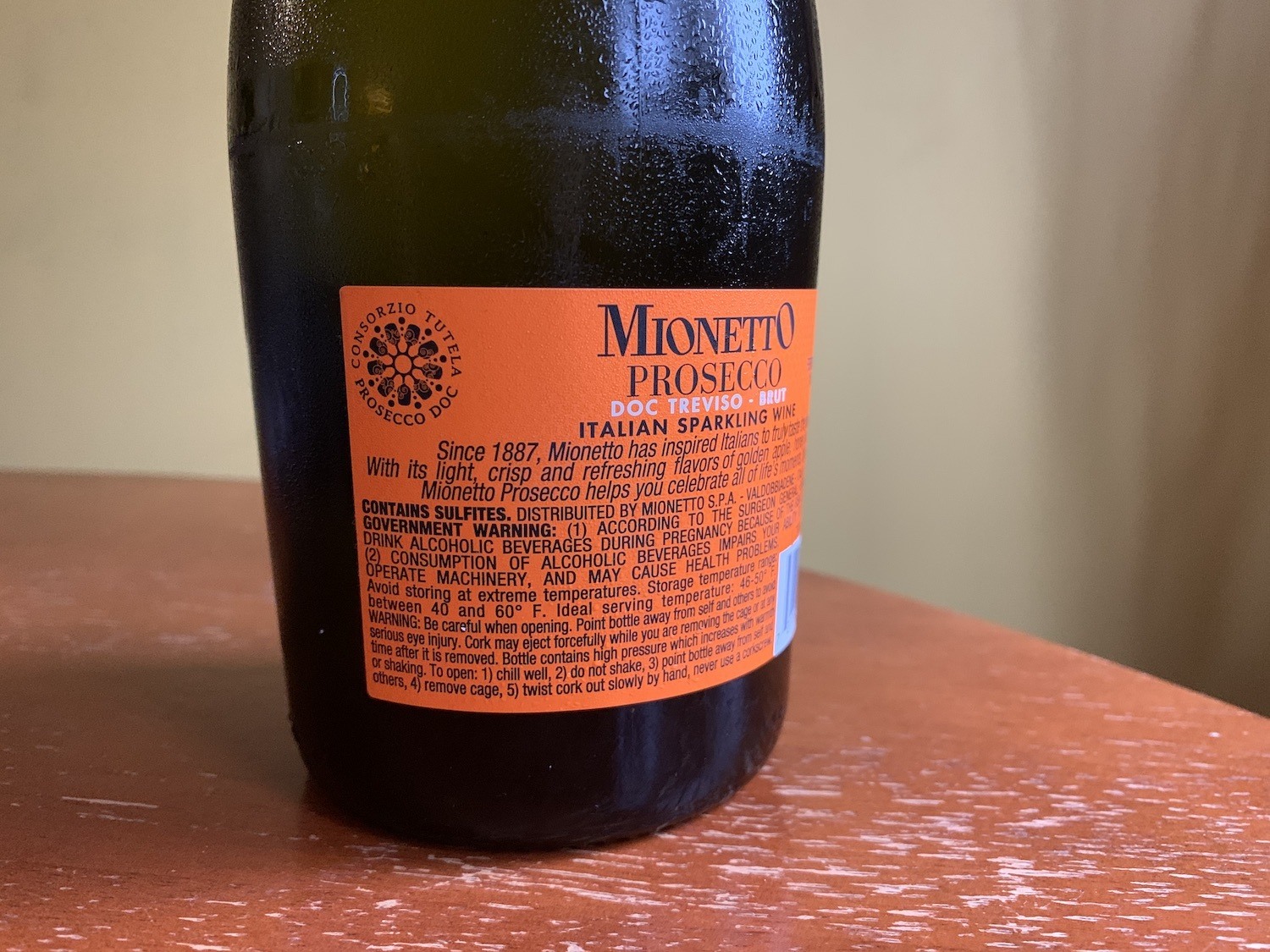
Since November 1989, federal law has required every alcoholic beverage bottle sold in the United States to bear a health message that warns pregnant women against drinking. However, the label has not been updated with new scientific findings since.
Talia Moore
That’s where cancer warnings can play a role, he added. Since November 1989, federal law has required every bottle of booze sold in the United States to bear a health message that warns pregnant women against drinking, and states that alcohol “may cause health problems.” However, the petition argues, this message hasn’t been updated in three decades and needs to be brought up to speed with the latest science. Gremillion says that the petition was inspired in part by Hobin and Stockwell’s study and it proposes a cancer warning identical to the one they used in Yukon. (In California, retailers must present alcohol cancer warnings to consumers at points of sale online and in stores, as required by Prop. 65. However, these are not required on products themselves, as such labeling falls under TTB oversight.)
The process to make those labels a mandated national reality, however, will require multiple steps. First, TTB has to recommend any proposed label changes to Congress. Lawmakers will then have to approve them. “That’s a big lift,” Gremillion admitted. And if the interruption of the Yukon experiment is any indication, alcohol lobby groups will likely pull out all the stops to prevent it from happening.
“I was surprised we were able to run it for [a month], honestly, before we got stopped,” said Stockwell, director of the Canadian Institute for Substance Use Research and professor of psychology at the University of Victoria. “I was thinking that that was only because it was in the Yukon, out in the middle of nowhere. Nobody quite knew what was going on until the launch—that’s why we got away with it.”
“On their own, well-designed labels can increase consumer knowledge of national drinking guidelines and serious, largely unknown alcohol-related health risks, such as cancer, as well as reduce per capita alcohol consumption.”
Despite the interruption, the team was able to pull a handful of telling findings from the cancer label’s four weeks in action: Shoppers in Whitehorse were significantly more likely to know about alcohol’s cancer risk than control groups. Researchers also found that total alcohol sales decreased by more than six percent. These findings were published in the Journal of Studies on Alcohol and Drugs in May.
“On their own, well-designed labels can increase consumer knowledge of national drinking guidelines and serious, largely unknown alcohol-related health risks, such as cancer, as well as reduce per capita alcohol consumption,” Hobin wrote in a email.
The U.S. petitioners will likely face tremendous pushback from the industry. Recently, for example, after a scientific advisory committee suggested in July that the next iteration of the Dietary Guidelines (DGA) lower its moderate drinking limit for men from two drinks per day to one—industry groups, their representatives, and lawmakers to whom the groups had poured hundreds of thousands in campaign contributions raised furor over the recommendation. They challenged its scientific basis, and in statements to the media, resuscitated the discredited idea that drinking can have health benefits.
“The alcohol industry is not doing anything different. They really see science as a threat to their viability.”
These marketing and lobbying efforts have been frequently compared to Big Tobacco’s old playbook on staving off public health regulations.
“The tobacco industry pioneered this by manipulating the science on heart disease and cancer, by hiring researchers who pretty much get on their payroll and then create doubt about the linkages,” said Thomas Babor, a professor of public health science at the University of Connecticut and the editor-in-chief of the Journal of Studies on Alcohol and Drugs. “The alcohol industry is not doing anything different. They really see science as a threat to their viability.”
And much like in the case of tobacco, public health advocates don’t expect the general public’s attitudes toward alcohol to shift overnight.
“[Alcohol] is a big part of our culture and of our society,” Hobin said. “Alcohol is present when we’re celebrating birthdays, weddings, anniversaries, in religious ceremonies. And because alcohol has been so prominent in our culture—that in and of itself creates a barrier because it’s been so normalized. In order to really start to rethink alcohol, it will take time and it will be gradual.”
“Those who know alcohol can cause cancer are 1.6 times more likely to support health warning labels relative to those who do not know.”
Right now, just two countries, South Korea and Ireland, have laws on the books requiring cancer warnings on booze. Gremillion’s hope for the Consumer Federation petition is that it also raises awareness of the alcohol-cancer link among the general public.
“A warning—and even short of that—just drawing attention to this could have a real, significant public health impact,” he said.
Down the line, widespread recognition may even result in greater pressure from drinkers themselves for cancer warnings. That might seem implausible, but Hobin and Stockwell’s study found that awareness is in fact linked to higher support for such messaging: “Those who know alcohol can cause cancer are 1.6 times more likely to support health warning labels relative to those who do not know,” the authors wrote.
Any industry pushback—and there undoubtedly will be industry pushback—might even incidentally serve the campaign’s interests. Just look at what happened with Hobin and Stockwell: When the industry pressured the Yukon government to halt their work, the move sparked vocal outrage and widespread coverage in both the domestic and international press. High-profile health columnist André Picard covered it, as did The New York Times and The Wall Street Journal. It wasn’t exactly the kind of exposure that researchers had expected, and it came with an unfamiliar degree of public esteem.
“I’m used to being unpopular talking about alcohol, because we all love our drink, and anyone who moans about how it’s bad for you, and that it should be restricted and so on can be very unpopular,” Stockwell said. “I got so much support.”







