Popular at-home food sensitivity tests may be misdiagnosing consumers
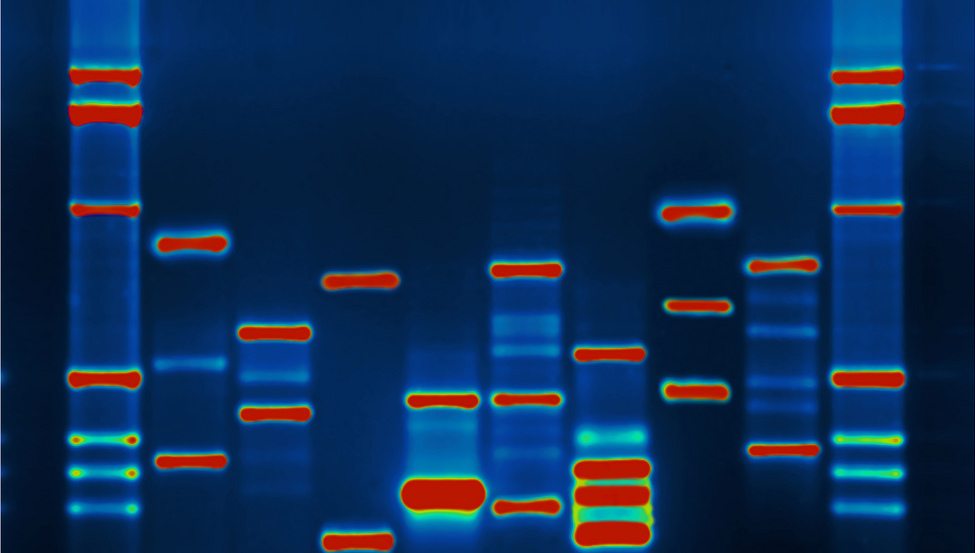
If you’re an even occasional TikTok scroller, chances are you’ve come across at least one video of someone raving—or ranting—about the results of a food sensitivity test. At-home tests kits, which use blood or hair samples to determine a person’s potential reactions to a dizzying array of foods, are the latest trend in the dieting world. But do they live up to the hype? At first glance, the kits seem more grounded in science than the “tests” my hippie mother used to subject me to as a child (I still don’t know where she got the idea that if you held a possibly offensive food item over your stomach with one hand and extended your other arm out from your body, someone could push down on the outstretched arm and diagnose an allergy by noting a decrease in strength in the arm. I spent most of my childhood subsisting on barley and tofu after my arm strength failed me on dairy, meat, rice, and everything in the cabbage family.) But I digress. The Wall Street Journal talked to dietitians about one of the most popular tests on the market today, which analyzes blood samples for immunoglobulin G (IgG) responses to nearly 100 foods. The dietitians were not impressed. Groups like the American Academy of Allergy, Asthma, and Immunology say that IgG testing is actually not backed by science. The jury is out on whether antibody levels can indicate a sensitivity—or actually, a tolerance—for food. In the meantime, dietitians are having to answer to anxious clients who have used these iffy at-home kits to self-diagnose. —Jessica Terrell